Source: NHPR – Paul Cuno-Booth
New Hampshire already faces a shortage of nursing assistants, home health aides and other direct care workers. But a state commission says thousands more will be needed as the population ages.
The New Hampshire Commission on Aging says strengthening that workforce — which helps people with disabilities and older adults manage daily tasks like meals, housekeeping and bathing — should be a top priority. Local advocates and an outside expert who recently testified before the commission say that will require higher wages and increases in state funding.
The direct care workforce was already a concern before the COVID-19 pandemic, when the “growing number of older adults, increased longevity, untenable low wages for caregivers, and shrinking number of people in the ‘working age’ cohort made this issue a brewing storm,” the advisory commission warned in its annual report, released Nov. 1.
Burnout and other issues during the pandemic further stressed the direct care workforce. According to the commission’s report, many older adults are not getting the care they need and are experiencing worse health outcomes because there are too few workers.
“People think if something happens to their loved one that they’ll, you know, make some calls, and there’ll be people to help them,” said Amy Moore, who directs an in-home care program serving New Hampshire at Ascentria Care Alliance. “And that’s not the case right now.”
The median direct care worker in New Hampshire earned $21,500 in 2020; a third of direct care workers relied on some form of public assistance.
According to PHI, a national policy organization focused on eldercare and disability services
While staffing has been a concern for years, she said the pandemic “made it a million times worse.”
Nearly all of her hires now are people who already know a client, like a neighbor or loved one, and are willing to go to work caring for them, she said. That often means giving up another job. She said other clients are forced to wait for the help they need because agencies like hers can’t hire enough caregivers, putting their health and safety at risk.
On Monday, the commission heard about strategies other states have used to build their workforces.
Amy Robins, director of advocacy for PHI, a national policy organization focused on eldercare and disability services, said a lot of solutions hinge on more funding. Low pay, poor benefits and limited paths for career advancement drive many people out of the field, she said.
“They work extraordinarily hard, many hours, and still have challenges paying their bills,” Robins said.
According to PHI, the median direct care worker in New Hampshire earned $21,500 in 2020; a third of direct care workers relied on some form of public assistance. Robins said those jobs are held disproportionately by women, people of color and immigrants in New Hampshire and nationally.
Robins said some states have raised minimum wages for direct care workers, required facilities to spend a certain percentage of revenue on care or invested in workforce training.
She said it’s also critical that states adequately fund Medicaid, which pays for a large portion of long-term care in the U.S., so that health care organizations have the resources to raise wages.
New Hampshire Health Care Association President and CEO Brendan Williams, whose organization represents long-term care facilities, hopes to see a substantial Medicaid increase in the next state budget. He said some nursing homes are leaving beds or whole wings empty because they can’t staff them, resulting in county nursing homes with waitlists of over 100 people.
“If there were actual closures of facilities, I think that would capture some headlines,” Williams told NHPR. “But what we’ve seen is equivalent to the closure of several facilities.”
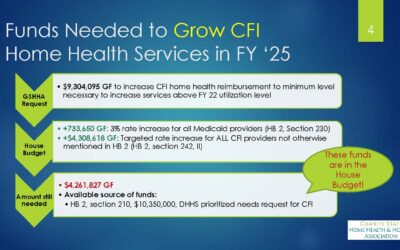
Moore said the rates the state pays for home-based supports, through a Medicaid-funded program known as Choices for Independence, are also too low. That makes it hard for agencies like hers to pay enough to attract and keep workers.
“There are actually a lot of people who want to do this work. As much as it’s challenging, it’s also super rewarding,” she said. “ … But no surprise, the pay is terrible.”
The Commission on Aging says it plans to make recommendations to the governor and legislature in the upcoming legislative session. It has identified areas of focus that include upping the rates for home-based care, expanding tuition assistance and training opportunities, and better marketing direct care as a career.