Source: Keene Sentinel
Borja Alvarez de Toledo says the home care workers he employs “perform miracles,” when they do the dressing, bathing and light housework that allows elderly adults, who are eligible for nursing home care, to continue to seek personal care services at home.
And yet, these workers are paid $13.50 an hour and are never eligible for benefits, said Alvarez de Toledo, CEO of Waypoint, a nonprofit agency that provides different social services throughout New Hampshire. The low wages and lack of benefits make it extremely difficult to find employees willing to provide this essential service.
“Obviously when we are not able to even pay what McDonald’s pays their workers, it’s really very complicated to recruit,” he said. “When we can’t recruit, there are seniors in need of very intensive care that don’t get the services they’re qualified for. There’s very little we can do.”
Each year, Waypoint loses roughly half a million dollars due to low Medicaid reimbursements from the state, according to Alvarez de Toledo.
Waypoint is not the only organization facing this reality.
Three nonprofits that spoke with The Sentinel said that because of New Hampshire’s low reimbursement rates on Medicaid-run home care programs, they are on the cusp of needing to suspend home care services, which allow people who qualify for nursing home-level of care to stay in their communities.
Already, the low availability of home care workers in New Hampshire means that some patients who wish to remain at home must live in nursing homes, while others wait for weeks in hospitals because it’s not safe for them to be discharged without home care support, experts say.
And both of those options end up costing the state more money than providing home care services, data show.
A July 2022 report from the N.H. Fiscal Policy Institute found that Choices for Independence (CFI) — a Medicaid waiver program that pays for home care for about 3,700 seniors of low income who are eligible for nursing-home level care in the state — has been underfunded by more than $153 million between 2011 and 2021, meaning that CFI needs almost $153 million to stay on par with current rates of inflation.
Underfunding for home care programs is an acute crisis, said Heather Carroll, advocacy director for the N.H. Alliance for Healthy Aging.
“Everybody talks about we’re heading off the cliff,” she said. “We’ve gone off the cliff.”
Low reimbursements contribute to a cycle of poverty, experts say
The underfunding of home care programs results in extremely low pay for workers, industry experts say.
In New Hampshire, the median wage for home health and personal care workers in 2021 was $14.12 an hour, according to the N.H. Fiscal Policy Institute. The statewide average wage that year for workers in all sectors was $30.12, according to the N.H. Employment Security, Economic and Labor Market Information Bureau.
“My daughter is 15 and makes more babysitting,” said Amy Moore, director of Ascentria In-Home Care, which provides services throughout the state, including in the Monadnock Region.
The population most adversely affected by the low hourly wage are Black, Indigenous, People of Color (BIPOC) folks and women.
National data from February 2022, show that 87 percent of direct care workers are women, 61 percent are people of color and 27 percent are immigrants. Home care workers are disproportionately Black, Hispanic, Asian American Pacific Islander and immigrants, according to a June 2022 report by the Economic Policy Institute, a D.C.-based think tank.
The low pay and lack of benefits is adversely impacting these populations, who are already facing barriers to pay equity. More than a quarter of direct care workers in New Hampshire are already living in poverty, according to PHI, a national organization focused on long-term care workers. Nationally, Latinx women earn the least at $23,500 a year on average, according to 2021 estimates.
Paying so little and not offering benefits like retirement and health insurance contributes to a cycle of poverty for home care workers, Alvarez de Toledo said.
The low pay and lack of benefits is entirely at odds with Toledo’s organization’s dedication to diversity, equity and inclusion — so much so that Alvarez de Toledo said that Waypoint will need to close, possibly as soon as the end of the year, if the state does not raise reimbursements, because he is unwilling to continue as is.
“We do not want to be complicit with the state in creating this subclass of employees,” he said.
Each state sets monthly reimbursements to agencies that provide care to residents who qualify for Medicaid.
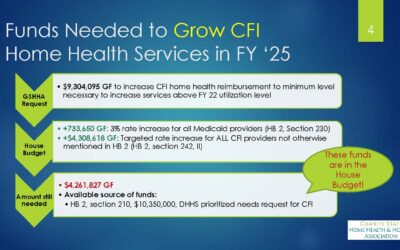
For many years, New Hampshire did not increase reimbursements for CFI at all, and the recent increases of roughly 3 percent annually since 2018 have “not kept up with inflation,” according to Gina Balkus, CEO of Granite State Home Health & Hospice Association. In 2021, the state budgeted $72.1 million for the CFI program, according to the N.H. Fiscal Policy Institute.
The long period of no reimbursement increase and steep inflation recently — over 5 percent this year — mean care workers are paid much less than other Granite State workers, Balkus said. It has also led to an ever-widening gap between New Hampshire’s annual CFI budget and the amount needed for CFI to keep on par with current inflation markers, according to the N.H. Fiscal Policy Institute.
In addition to the chronic underfunding, state officials acknowledge that providers lose money on Medicaid programs.
For example, it costs agencies about $79 per visit in 2020 for a home health aide to visit a patient. This amount factors in travel, supervision and other administrative costs, Balkus said. Medicaid reimburses that service at $34.68 for a visit lasting less than two hours. The idea is that profits from services billed to private insurance companies will cover the gap, a concept known as “cost shifting.”
Home Healthcare, Hospice and Community Services (HCS) — which has offices in Keene, Peterborough and Charlestown — is faring better than many other home care providers in the state because of cost shifting.
“We have the good fortune of being fully staffed,” said CEO Maura McQueeney, noting that HCS pays home care workers $23 an hour and provides benefits.
However, she emphasized that HCS still loses money providing home care through CFI and other Medicaid-funded programs. It’s only able to cover those costs by distributing overhead like costs for administrators and employee benefits with other programs that are paid for by the state and private insurers, or relies on charitable donations, which she said make up 6 percent of HCS’s annual operating budget.
At many agencies, like Waypoint and Ascentria, the majority of patients are on Medicaid, so the whole concept of cost shifting falls apart, providers say. Even with a healthy workforce, HCS is considering if it’s sustainable to continue providing home care through Medicaid-funded programs, McQueeney said.
“There are programs that drain our resources at a faster rate, to deliver services to a smaller number of people,” she said. HCS “can’t afford to take more [Medicaid-funded home care] patients, because each patient represents a loss … If we were to accept more, we would be infringing on the other programs.”
The low wages and workforce shortage ultimately result in elderly and disabled patients not getting the care they are entitled to, experts say. In 2022, only 66 percent of approved services under the CFI program were delivered, according to Balkus. Without Medicaid, home care costs in New Hampshire are higher than the national average. New Hampshire seniors also pay $1,406 more than the national average of $4,957 in home care services monthly.
At Ascentria, Moore said, 50 to 100 new patients are turned away each week. Case managers regularly shuffle patients to try to ensure everyone gets at least some care because there’s no way to meet the full need.
“You’re moving people around to just do the bare minimum, rather than people getting what they’re supposed to get for care,” Moore said.
The Keene-based N.H. Care Collaborative provides case management for CFI patients around the state, including in the Monadnock Region. When a person is approved for home care, a team of case managers calls local agencies to try to find workers to provide the hours, according to Jena Rutter, director of CFI at the Care Collaborative.
“We ask them all at the same time and hope for the best …,” Rutter said. “It’s usually a no.”
When Rutter can’t find a home care worker for a patient, she said, the patient is put on a waitlist. But in reality, she said that doesn’t mean much, with available care hours so hard to come by.
“We lose clients because they have to go into a nursing facility,” Rutter said. “Or, they end up in the hospital and the hospital can’t safely discharge them, and then we have no beds at the hospital. It’s like this circle.”
Once in the hospital, a patient who requires home care can’t be discharged until there’s a home care or nursing care plan in place. With few workers available, patients are often left waiting in the hospital, even when they don’t need that level of care.
Currently at Cheshire Medical Center in Keene, about 20 percent of patients are awaiting safe discharge, according to Chief Financial Officer Dan Gross.
“The beds they occupy means that we have one less bed for a patient who needs care,” Gross said in an email. The prolonged use of hospital beds leads to longer emergency-room wait-periods and an inability to admit new patients, Gross added.
At Dartmouth Hitchcock Medical Center in Lebanon, about 15 percent of patients have been in the hospital for more than 20 days, according to Colin D. Stack, medical director of the hospital’s capacity coordination center.
“Many of them are ready for discharge and simply lack a safe or appropriate place to go for the next phase of their care,” he said.
Like at Cheshire Medical, Stack said lack of home care providers limits the medical center’s ability to accept new patients, including those who need transfers from regional partners like Cheshire.
When patients need to rely on hospital stays or nursing home care, the state has to pay more for that service. Nursing home care in New Hampshire costs $98,111 annually, compared to $18,997 for the CFI program, according to the N.H. Fiscal Policy Institute. Hospital care is even more expensive, according to Balkus. A day of hospital care costs about $10,000 on average, federal data show.
“If it doesn’t hit people from the stories and moral obligation, you can just look at it from the financial standpoint,” Moore said. “[Home care] is so much more cost effective than institutionalizing people.”
New Hampshire has fallen behind other states in home care spending
New Hampshire was an early adopter for a few home care programs, according to Sletten. But, recent data show that New Hampshire spends less on home and community-based services than neighboring states such as Massachusetts, Vermont and Maine. This suggests that the Granite State relies more on nursing homes than on more affordable home care, Sletten said.
In 2019, the Granite State spent only 41 percent of the total Medicaid funding for long-term care on home and community based services, according to data from the N.H. Fiscal Policy Institute.
The majority of this funding was used to pay for nursing home care. The same year, Maine spent 64 percent on home care, Vermont spent 68 percent, and Massachusetts spent 72 percent of long-term care funding on home and community-based programs.
The variation in wages for home care workers in different states not only impacts patients, but also reduces the home care workforce in New Hampshire, where pay is significantly lower, experts say.
The issue is particularly acute in areas like the Monadnock Region that border other states. Since neighboring states have higher reimbursements, agencies are able to pay workers more. For the lowest paid home care workers, who make an average of $11.56 an hour in New Hampshire, taking the same job over the border in Massachusetts would result in a 23.6 percent annual wage increase.
“There’s an erosion around the borders,” Carroll said. “We have a well-trained valuable workforce that is now being poached by other states.”
There’s also an inequitable distribution of services within New Hampshire. Rural communities, like Antrim and Hillsboro, are often the most difficult to find caregivers for, according to Alvarez de Toledo. At the same time, because of driving distances, he said, those are the communities where it’s most expensive to provide care.
In addition, Medicaid isn’t available to everyone. While citizens of low income and permanent residents are eligible for Medicaid, the program leaves behind certain noncitizen immigrants and undocumented residents, including people on Deferred Action for Childhood Arrivals (DACA).
McQueeney, of HCS, is afraid that without adequate funding, national businesses that have “the luxury of scale and centralized operations” will take over home care in New Hampshire if the service is no longer sustainable for local organizations like hers.
Not having local providers would be a loss, she said, because there’s a certain flexibility that comes with a provider with strong community ties.
“There is something to be valued and retained in having an independent health care provider who doesn’t need to check the rule book to see if they can come out for one more visit,” she said. “People need to consider … what does it mean to be a community?”
For providers, including Madeline Ullrich, executive director of the N.H. Care Collaborative, the solution is simple: higher reimbursements for home care services, so that workers can earn a livable wage and patients can get the care they’re entitled to.
“New Hampshire knows what to do,” she said. “They need to get paid more money.”
Gaps in home care
With low wages and few workers, NH home care system has ‘gone off the cliff.’
Borja Alvarez de Toledo says the home care workers he employs “perform miracles,” when they do the dressing, bathing and light housework that allows elderly adults, who are eligible for nursing home care, to continue to seek personal care services at home.
And yet, these workers are paid $13.50 an hour and are never eligible for benefits, said Alvarez de Toledo, CEO of Waypoint, a nonprofit agency that provides different social services throughout New Hampshire. The low wages and lack of benefits make it extremely difficult to find employees willing to provide this essential service.
Paying so little and not offering benefits like retirement and health insurance contributes to a cycle of poverty for home care workers, Alvarez de Toledo said.
Home Healthcare, Hospice and Community Services (HCS) — which has offices in Keene, Peterborough and Charlestown — is faring better than many other home care providers in the state because of cost shifting.
“We have the good fortune of being fully staffed,” said CEO Maura McQueeney, noting that HCS pays home care workers $23 an hour and provides benefits.
However, she emphasized that HCS still loses money providing home care through CFI and other Medicaid-funded programs. It’s only able to cover those costs by distributing overhead like costs for administrators and employee benefits with other programs that are paid for by the state and private insurers, or relies on charitable donations, which she said make up 6 percent of HCS’s annual operating budget.